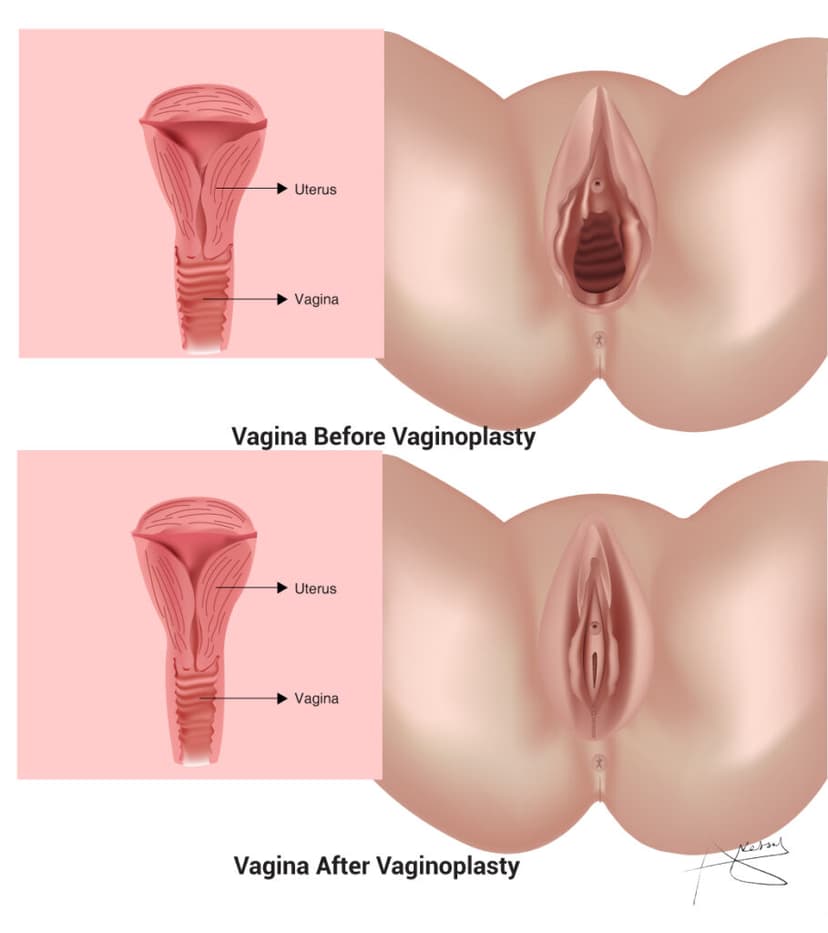
Vaginoplasty is a surgical procedure that involves the construction or reconstruction of the vagina. It is a type of gender-affirming surgery sought by some transgender women as part of their transition, but it can also be performed for other medical reasons, such as to repair congenital anomalies or following trauma or cancer treatments. For transgender women, vaginoplasty is often performed as part of gender confirmation surgery to align their physical characteristics with their gender identity. The procedure typically involves creating a neovagina using existing penile and scrotal tissue, and sometimes additional tissue grafts may be used. The surgeon will reshape the tissue to form the vaginal canal, and the procedure may also include the creation of a clitoral hood and labia
- Consultation and Evaluation: Before the surgery, the individual will have multiple consultations with a qualified surgeon specializing in gender-affirming surgeries. The surgeon will evaluate the individual's medical history, perform a physical examination, and discuss their expectations and goals for the procedure.
- Preparation: In the weeks leading up to the surgery, the individual may be required to stop taking certain medications that could increase the risk of bleeding and complications during surgery. They may also be advised to stop smoking, as smoking can impair healing
- Anesthesia: Vaginoplasty is typically performed under general anesthesia, which means the individual will be asleep and won't feel any pain during the surgery.
- Incision: The surgeon will make an incision between the scrotum and the anus. The scrotal tissue will be used to create the vaginal canal, and the penile tissue may be used to form the labia.
- Vaginal Canal Creation: The surgeon will carefully remove the erectile tissue from the penis while preserving the nerve and blood supply. This tissue is then used to create the inner lining of the vaginal canal.
- Labia Formation: The scrotal skin is used to create the labia minora and majora, which are the outer lips of the vagina.
- Clitoral Hood Construction: The head of the penis (glans) is often preserved and used to create a clitoral hood, giving the neovagina a more natural appearance
- Suturing: The surgeon will carefully suture the tissues together to create the new vaginal canal and external genitalia
- Dressings and Catheter: After the surgery, dressings are applied to protect the surgical site, and a catheter is inserted into the urethra to drain urine from the bladder.
- Recovery: The individual will be closely monitored during the initial recovery period. Pain management and wound care will be provided, and the catheter will remain in place until the healing process progresses sufficiently.
- Follow-up Care: After discharge, regular follow-up appointments with the surgeon will be scheduled to monitor healing progress and address any potential complications.
- Gender Affirmation: For transgender women, vaginoplasty can be a crucial step in their gender affirmation journey. It helps align their physical appearance with their gender identity, reducing gender dysphoria and improving their overall well-being and mental health.
- Improved Quality of Life: For individuals with congenital anomalies or conditions like vaginal agenesis or stenosis, vaginoplasty can greatly improve their quality of life. It can enhance sexual function, allow for more comfortable and enjoyable sexual activity, and enable menstruation in cases where it was not possible before.
- Psychological Well-being: Vaginoplasty can have a positive impact on an individual's psychological well-being, leading to increased self-confidence, body satisfaction, and improved body image. This can result in better overall mental health and a greater sense of selfacceptance
- Sexual Function: For many transgender women and individuals with vaginal anomalies, vaginoplasty can lead to the development of a functional and sensate neovagina. Although the level of sensation can vary between individuals, many report being able to experience sexual pleasure and arousal after the procedure.
- Reduction in Gender Dysphoria: For transgender women, vaginoplasty can significantly reduce gender dysphoria associated with the misalignment between their gender identity and their external genitalia. This can lead to a more authentic and fulfilling life
- Social and Cultural Integration: Vaginoplasty can help transgender women integrate more comfortably into social and cultural settings that expect a certain level of congruence between gender identity and physical appearance
- Congenital Anomalies: Some individuals are born with congenital conditions that affect the development of the vagina or reproductive organs. Vaginoplasty can be performed to create or reconstruct the vaginal canal, helping to correct these anomalies and improve the individual's quality of life.
- Vaginal Agenesis or Absence: Vaginal agenesis is a condition in which the vagina does not fully develop or is absent. This condition can cause difficulties with menstruation, sexual activity, and psychological distress. Vaginoplasty can be used to create a functional vaginal canal in individuals with this condition.
- Vaginal Stenosis: Vaginal stenosis refers to a narrowing or constriction of the vaginal canal. This condition can occur due to scarring from previous surgeries, radiation therapy, or other medical reasons. Vaginoplasty can be used to widen and reconstruct the vaginal canal, improving sexual function and quality of life.
- Gender-Affirming Procedures for Non-binary and Gender Non-conforming Individuals: Some non-binary and gender non-conforming individuals may also choose to undergo vaginoplasty as part of their gender-affirming journey. The decision to undergo the procedure is a deeply personal one, and it can help alleviate gender dysphoria and improve well-being.
- Pain and Discomfort: Pain and discomfort are common during the initial stages of recovery. The surgical site may be swollen and tender, and pain medications prescribed by the surgeon will help manage any discomfort
- Wound Care: Proper wound care is essential for preventing infections and promoting healing. The surgical site will be dressed and may require regular cleaning and changing of dressings during the early recovery period.
- Catheter: A catheter is often used to drain urine from the bladder in the immediate post-operative period. The catheter is usually removed after a week or so once the individual can urinate independently
- Restricted Activities: Physical activity and strenuous movements should be avoided during the early recovery period. The surgeon will provide guidelines on activity restrictions, which may include avoiding heavy lifting and sexual activity for a specified period.
- Dilations: Regular dilation of the neovaginal canal is a crucial part of the recovery process. Dilations help prevent narrowing (stenosis) of the newly created vaginal canal and maintain its depth and width. The surgeon will provide instructions on the frequency and technique for dilation.
- Follow-up Appointments: Regular follow-up appointments with the surgeon are essential during the recovery period. These appointments allow the surgeon to monitor healing progress, address any concerns, and provide guidance on the recovery process.
- Return to Work and Normal Activities: The timing for returning to work and normal daily activities will depend on the individual's healing progress and the nature of their job. Many individuals can expect to take several weeks off from work to focus on recovery
- Swelling and Bruising: Swelling and bruising are common after surgery and will gradually subside over time
- Emotional Support: Emotional support from friends, family, or support groups can be beneficial during the recovery period. It is normal to experience a range of emotions during this time, and having a support network can make the process more manageable.
- Doctor Fees
- OT charges
- Anesthetic charges
- Drugs
- Investigation
- Professional charges
- Room Rents
- Nursing & Administrative charges